Abstract
Introduction: Hyperleukocytosis at time of acute myeloid leukemia (AML) diagnosis is associated with increased disease-related complications as well as early mortality. Many AML patients are not candidates for intensive chemotherapy (IC) because of disease-related or patient-specific factors. Limited data is available regarding the characteristics and outcomes of newly-diagnosed AML who present with hyperleukocytosis and do not receive IC.
Methods: We retrospectively analyzed data from patients with newly-diagnosed AML and hyperleukocytosis (defined as white blood cell count [WBC] of 50 × 109/L or greater) who were reported not to have received IC at 12 major institutions in the United States, Spain, Germany and France from 1982 to the end of 2016. Collected variables included age, sex, Eastern Cooperative Oncology Group Performance Status (ECOG PS), WBC, hemoglobin level, platelet count, renal and hepatic chemistry parameters, cytogenetic risk group, molecular abnormalities (if available), presence of tumor lysis syndrome (TLS), disseminated intravascular coagulation (DIC), clinical evidence of leukostasis, admission to an intensive care unit (ICU) at presentation, receipt of hydroxyurea, and administration of leukapheresis. Clinical evidence of leukostasis was defined as new onset hypoxia, chest pain, headache, focal neurological symptoms, priapism, intestinal ischemia and acute renal failure attributed to hyperleukocytosis by the primary provider of the patient. Kaplan-Meier analysis was used to estimate overall survival (OS) from time of presentation until death or end of follow-up. Patients with hyperleukocytosis who received IC are described in a separate abstract.
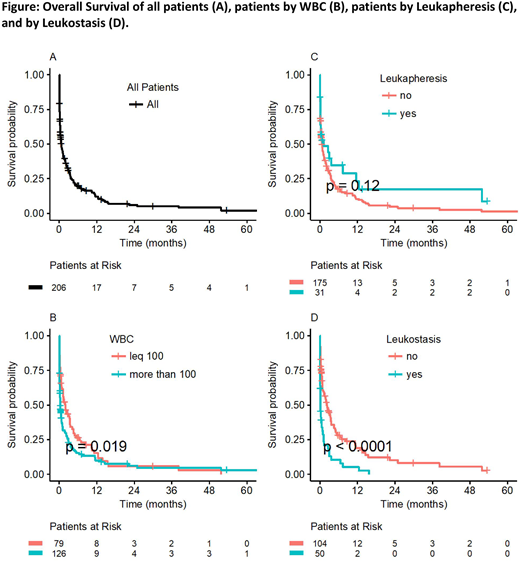
Results: Of 1050 patients with AML and hyperleukocytosis reported to our dataset, 220 patients were reported not to have received IC and were included in this analysis. For those 220 patients, median age was 75 years, 57.7% were male, and most (62.8%) had an ECOG PS of 2 or greater. Median WBC, hemoglobin, and platelet count at presentation were 131.4 × 109/L (range [R], 50.4-620), 8.96 g/dL (R, 3.6-15.9), and 34 (R, 3-393), respectively; 61.5% presented with a WBC greater than 100 × 109/L. Cytogenetically-defined poor risk AML was diagnosed in 26.1% of patients. TLS, DIC or clinical leukostasis was present in 25.6%, 15.7%, and 32.5% of patients, respectively. Pulmonary, central nervous system, renal, cardiac, gastrointestinal, or retinal clinical evidence of leukostasis was present in 52.9%, 17.1%, 11.4%, 10%, 5.7% and 2.9%, respectively, of those with clinical leukostasis. The majority (72.9%) of patients received initial therapy with hydroxyurea with a median time from presentation to administration of 12 hours (R, 1-144). Only 15% of patients underwent leukapheresis. Commonly-used non-IC therapies included hypomethylating agents, clofarabine, low dose cytarabine, or best supportive care. The median OS of the entire cohort was only 22 (95%CI: 13-37) days. The 30-day mortality was 57.4%. The 60-day, 90-day, 180-day, and one-year OS probabilities were 37%, 31%, 20%, and 12%, respectively. Only 4.3% of patients proceeded to allogeneic stem cell transplant. Patients presenting with WBC >100 × 109/L (N=79) had a worse OS than those presenting with WBC <100 × 109/L (N=126), (median OS 0.4 [95%CI, 0.3-0.7] vs. 2 [95%CI, 1.2-3.5] months, respectively, p=0.02) and those with clinical evidence of leukostasis (N=50) had worse OS than those who did not (N=104), (median OS, 0.2 [95%CI, 0.1-0.8] vs 2.2 [95%CI, 1.3-3.5] months, respectively, p<0.0001) (Figure). Patients who underwent leukapheresis (N=31) did not have a significantly improved OS compared to those who did not undergo leukapheresis (N=175) with a median OS of 1.2 (95%CI, 0.2-12.4) vs. 0.7 (95%CI, 0.4-1.2) months, respectively (p=0.12) (Figure). The small number of patients undergoing leukapheresis limited assessment of impact of leukapheresis in multivariable analysis.
Conclusions: We report the largest studied cohort of patients with newly-diagnosed AML presenting with hyperleukocytosis who did not receive IC. Outcomes were very poor with a median OS of 22 days and only 12% alive at one year. WBC >100K x 109/L and clinical leukostasis were associated with inferior survival, while leukapheresis did not seem to impact survival. Novel and effective therapies are urgently needed for this group of AML patients.
Montesinos:Daiichi Sankyo: Consultancy, Speakers Bureau; Novartis: Research Funding, Speakers Bureau. Bhatt:Incyte: Research Funding; CSL Behring: Consultancy; Pfizer: Consultancy. Sekeres:Opsona: Membership on an entity's Board of Directors or advisory committees; Opsona: Membership on an entity's Board of Directors or advisory committees; Celgene: Membership on an entity's Board of Directors or advisory committees; Celgene: Membership on an entity's Board of Directors or advisory committees. Fathi:Agios: Honoraria, Research Funding; Astellas: Honoraria; Boston Biomedical: Consultancy, Honoraria; Celgene: Consultancy, Honoraria, Research Funding; Jazz: Honoraria; Seattle Genetics: Consultancy, Honoraria; Takeda: Consultancy, Honoraria. Khan:Teva: Speakers Bureau. Roboz:AbbVie: Consultancy; Cellectis: Research Funding; Celltrion: Consultancy; Argenx: Consultancy; Aphivena Therapeutics: Consultancy; Eisai: Consultancy; Novartis: Consultancy; Otsuka: Consultancy; Astex Pharmaceuticals: Consultancy; Bayer: Consultancy; Celgene Corporation: Consultancy; Cellectis: Research Funding; Roche/Genentech: Consultancy; Roche/Genentech: Consultancy; Eisai: Consultancy; Aphivena Therapeutics: Consultancy; Otsuka: Consultancy; Pfizer: Consultancy; Sandoz: Consultancy; Sandoz: Consultancy; Orsenix: Consultancy; AbbVie: Consultancy; Janssen Pharmaceuticals: Consultancy; Astex Pharmaceuticals: Consultancy; Celltrion: Consultancy; Janssen Pharmaceuticals: Consultancy; Jazz Pharmaceuticals: Consultancy; Celgene Corporation: Consultancy; Orsenix: Consultancy; Jazz Pharmaceuticals: Consultancy; Daiichi Sankyo: Consultancy; Novartis: Consultancy; Bayer: Consultancy; Daiichi Sankyo: Consultancy; Pfizer: Consultancy; Argenx: Consultancy. Cluzeau:Pfizer: Speakers Bureau; Sanofi: Speakers Bureau; AbbVie: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Amgen: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Jazz Pharma: Consultancy, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Menarini: Consultancy; Celgene: Consultancy, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau. Germing:Celgene: Honoraria, Research Funding; Janssen: Honoraria; Novartis: Honoraria, Research Funding. Mukherjee:Takeda: Membership on an entity's Board of Directors or advisory committees; Takeda Pharmaceuticals: Membership on an entity's Board of Directors or advisory committees; Projects in Knowledge: Honoraria; Pfizer: Honoraria; Novartis: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding; LEK Consulting: Consultancy, Honoraria; Bristol Myers Squib: Honoraria, Speakers Bureau; BioPharm Communications: Consultancy; Aplastic Anemia & MDS International Foundation in Joint Partnership with Cleveland Clinic Taussig Cancer Institute: Honoraria. Brunner:Celgene: Consultancy, Research Funding; Takeda: Research Funding; Novartis: Research Funding. Ritchie:NS Pharma: Research Funding; Incyte: Consultancy, Speakers Bureau; Novartis: Consultancy, Other: Travel, Accommodations, Expenses, Research Funding, Speakers Bureau; Astellas Pharma: Research Funding; Bristol-Myers Squibb: Research Funding; ARIAD Pharmaceuticals: Speakers Bureau; Pfizer: Consultancy, Research Funding; Celgene: Consultancy, Other: Travel, Accommodations, Expenses, Speakers Bureau. Podoltsev:Astex Pharmaceuticals: Research Funding; Celator: Research Funding; Astellas Pharma: Research Funding; Daiichi Sankyo: Research Funding; Sunesis Pharmaceuticals: Research Funding; Boehringer Ingelheim: Research Funding; CTI biopharma: Research Funding; Celgene: Research Funding; Pfizer: Consultancy, Honoraria, Research Funding; Alexion: Consultancy, Honoraria. Gore:Celgene: Consultancy, Research Funding. Zeidan:Otsuka: Consultancy, Honoraria; Celgene: Consultancy, Honoraria; Pfizer: Consultancy, Honoraria; Novartis: Consultancy, Honoraria; AbbVie: Consultancy, Honoraria; Takeda: Honoraria, Speakers Bureau; Agios: Consultancy, Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal